The research program coordinated by Paolo Macor is centred on the development of new therapeutic approaches. The pivotal aim of these strategies is to allow the delivery of a drug (recombinant antibody, chemotherapeutic agents, anti-miRNA, siRNA, DNA vectors or aptamers) to specific microenvironment in order to enhance the therapeutic effect increasing the local doses but reducing the side effects caused by the general distribution of the drug. Moreover Paolo Macor is an expert in the study of the pathophysiological role of the complement system.
All the activities within this program are organized in 2 main lines of research. One is devoted to the development of targeted nanoparticles for the diagnosis and the treatment of B-cell malignancies, like Non-Hodgkin lymphoma and chronic lymphocytic leukemia; the second one is dedicated to the characterization of targeted recombinant antibodies and targeted nanoparticles for the treatment of inflammatory diseases like rheumatoid arthritis.
1. Treatment of B-cell malignancies
1.1 Development of anti-CD20 bicompatible/biodegradebla polymeric nanoparticles
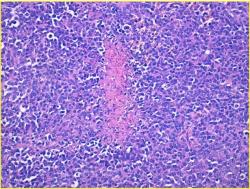
B-cell malignancies are a heterogeneous group of clinical conditions with high variability. Current B-cell disorder treatments take advantage of dose-intensive chemotherapy regimens and immunotherapy via use of monoclonal antibodies. Unfortunately, they may lead to insufficient tumor distribution of therapeutic agents, and often cause adverse effects on patients. Due to the cytotoxicity of drugs, currently the major challenge is to deliver the therapeutic agent to neoplastic cells while preserving the viability of non-malignant cells.
Our team proposes a new therapeutic approach in which high doses of chemotherapeutic drug were loaded into biodegradable polymeric nanoparticles coated with an anti-CD20 antibody. We demonstrate their ability to target and internalize in tumor B-cells. Moreover, these nanoparticles were able to kill tumor B-cell lines, but also circulating primary cells expressing a low amount of CD20 and purified from leukemic patients. Their safety and their efficacy were demonstrated in models reproducing the clinical features of the pathologies.
The plasticity of the polymeric nanoparticles allows to load active molecules with different nature, such as recombinant antibodies, chemotherapeutic agents, anti-miRNA, siRNA, DNA vectors or aptamers. Several particles has been developed in our laboratories, loaded with fludarabine, bendamustine, anti-miR17, aptamers or siRNA blocking the protein eEF1A1, boron, or vectors encoding for luciferin, GFP and other proteins.
The specificity of targeted particles to tumor B-cells suggests the use of anti-CD20 nanoparticles as diagnostic tools to visualize tumor masses. To this end specific probes, like cynin5.5, gadolinium-complexes or iron-complexes, were loaded in targeted particles analyzed using near-infrared optical imaging, NMR and CT.
Although this approach is devised for treatment of B-cell malignancies, this strategy can easily be applied to different types of tumors, using other targeting agents to specifically deliver cytotoxic drug-loaded nanoparticles in cancer cells.
In these studies are involved different groups and companies: LNK Chemsolutions LLC (Lincoln, NE, USA), Bio-Target Inc (Chicago, IL, USA), CUCAIBA (Ministry of Health, La Plata, Buenos Aires, Argentina), Clinical and Experimental Onco-Hematology Unit, Centro di Riferimento Oncologico (I.R.C.C.S., Aviano, Italy), Department of Human Pathology, University of Palermo (Palermo, Italy).
1.2 Development of bispecific antibodies able to bind CD20 and to neutralize membrane complement regulatory proteins
Current strategies for cancer therapy with monoclonal antibodies (mAb) are mainly based on targeting proteins expressed on the surface of cancer cells that are easily accessible. These antibodies exert anti-neoplastic effects either by inducing apoptosis or by engaging immune effector mechanisms, such as Ab-dependent cellular cytotoxicity (ADCC), Ab-dependent cellular phagocytosis and complement-dependent cytotoxicity (CDC). Despite the advantages of the complement system (C) in the control of tumor growth, very few studies are based on methods that enhance C-mediated functions. The major limitation of C-mediated tumor cell lysis is the overexpression of the C-regulatory proteins CD46, CD55 and CD59 on the cell surface (mCRPs). These proteins permit evasion of complement attack and restricts the complement-dependent cytotoxic effect of several antibodies.
We generated two bispecific recombinant antibodies (bsAbs) that were designed to recognize CD20 and to neutralize the CD55 or CD59.
The choice to neutralize CD55 and CD59 was based on our previous observations. We have demonstrated that these two C regulators contribute to the protection of CD20+ B-lymphoma cells from complement-mediated killing induced by the anti-CD20 mAb rituximab.
Our data show that treatment with a mixture of the two bsAbs targeting CD20 on B-lymphoma cells prevents tumor development and results in the survival of all tumor-bearing animals.
This approach was devised for the generation of bsAbs carrying the specificity of the anti-CD20 Ab rituximab, but this strategy can easily be applied the other antitumor C-fixing antibodies currently used in the clinic or tested in preclinical studies using the same vector with the appropriate modifications.
In these studies are involved different groups: Clinical and Experimental Onco-Hematology Unit, Centro di Riferimento Oncologico (I.R.C.C.S., Aviano, Italy), Department of Human Pathology, University of Palermo (Palermo, Italy), Department of Health Sciences and IRCAD, University of Eastern Piedmont (Novara, Italy), Institute for Maternal and Child Health–IRCCS ‘Burlo Garofolo’ (Trieste, Italy).
2. Treatment of rheumatoid arthritis
2.1 Development of nanoparticles specific for inflamed synovial tissue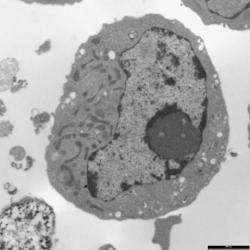
Rheumatoid arthritis (RA) is an autoimmune disease characterized by chronic inflammation of synovial tissue, leading to cartilage destruction and bone erosion and causing the major clinical symptoms associated with RA like joint swelling and deformities, stiffness and pain. Nowadays, methotrexate is the most common drug used to treat RA patients. Due to its toxicity into high proliferative cells, it was originally developed to treat cancer and then was also used to treat autoimmune diseases. Despite the success of the treatment of rheumatoid arthritis, many patients fail to respond to the available therapies and true remission is achieved only by a minority. This is also due to a late diagnosis of the pathology. Moreover, the currently available therapies used to treat RA cause several side effects. There is therefore the need to develop a new tool for an early diagnosis of the disease but also to develop tissue specific agents able to reduce systemic side effects, increasing the potency of the drug using lower doses.
The idea is to use biodegradable polymeric nanoparticles (BNPs) coated by a previously described homing-peptide specific for inflamed synovial tissue in order to:
- drive into inflamed synovium BNPs filled by contrast agents (gadolinium or iron complexes) as a diagnostic tool for an early and functional diagnosis of joint inflammation
- drive only into arthritic synovium BNPs loaded with methotrexate as a therapeutic agents.
A complete preclinical study of these potential an diagnostic and therapeutic tools will be performed.
In these studies are involved different groups and companies: LNK Chemsolutions LLC (Lincoln, NE, USA), Bio-Target Inc (Chicago, IL, USA), Istituto Auxologico Italiano IRCCS (Milan, Italy), Department of Clinical Sciences and Community Health, University of Milan (Milan, Italy), Department of Human Pathology, University of Palermo (Palermo, Italy).
2.2 Development of targeted recombinant antibody specific for inflamed synovial tissue
Rheumatoid arthritis (RA) is a chronic, progressive, inflammatory autoimmune disease. T cells, B cells and the orchestrated interaction of pro-inflammatory cytokines play key roles in the pathobiology of RA. TNF is clearly of primary importance in the pathogenesis of RA and was the first cytokine to be fully validated as a therapeutic target for RA. Although the favorable efficacy profile of anti-TNF antibodies is promising, they are not without limitations and several potential clinical challenges, most notably safety, may be associated with their use. One innovative strategy for simultaneously lowering both the side effects and the cost is to deliver selectively the drug to inflamed synovium. We propose an alternative approach that was taken following the identification of a peptide that binds selectively to synovial microvascular endothelium with a selective accumulation of the drug at tissue level thus avoiding side effect that may derive from long-term systemic administration of therapeutic drugs.
Targeted anti-TNF-α neutralizing antibody was already prepared in our laboratory and its initial characterization demonstrated its potential efficacy.
3. Treatment of inflammatory bowel disease
3.1 oraCle: New integrated approach to oral therapy of Crohn’s disease
oraCle is a project funded by the Autonomous Region of Friuli Venezia Giulia within the POR FESR 2014-2020, activity 1.3.b, aimed at studying a new integrated approach to oral therapy of Crohn’s disease (Contribution granted: Euro 877,360.29)
Crohn’s Disease: up to date
Crohn’s Disease (CD) is an idiopathic autoimmune disease of the digestive tract that mainly affects the ileum and the colon. Symptoms (abdominal pain, diarrhoea, weight loss, flu-like syndrome) and complications, both intestinal and extraintestinal, have a serious impact on the life quality patients, who are mostly young (10-25 years). The rate of incidence, ranging from 150 to 200 cases per 200,000 people, is unfortunately growing, especially in patients of pediatric age To date, classical corticosteroid treatments are not able to alter the evolution of the disease, but can only control the inflammatory state. Only monoclonal antibody therapy, against TNF alpha has been able to revolutionize the patients’ lives, giving them, however, severe side effects.
The aim of the oraCle project is to create a therapy that carries the anti-TNF alpha antibodies directly to the intestine, both avoiding patient’s immunosuppression caused by the systemic exposure and maintaining its therapeutic efficacy.
PROJECT PARTNERS AND PLANNED ACTIVITIES
Transactiva Srl, a biotech company specialized in molecular farming of therapeutic proteins in plants, intends to produce the anti-TNF alpha antibody in rice seeds. The purified protein will be used in combination with the probiotic Kluyveromyces marxianus fragilis (TURVAL B0399) produced by Turval Laboratories Srl to develope an innovative oral therapy. Recent studies demonstrate that probiotics improve the digestive functions, the treatment and the prevention of recurrences in people with irritable bowel syndrome. The choice of gastroresistant capsules and excipients, essential elements for the protection of the active substances and their controlled release into the intestine, will be carried out by Biofarma Spa, a leader in the production of food supplements, medical devices and cosmetics. The University of Udine will evaluate the antibody’s bioactivity, protected by different matrixes, to the chemical, enzymatic and microbiological treatments using in vitro models of the digestive system, while the therapeutic efficacy will be evaluated in vivo by the University of Trieste thanks to an animal model that mimics Crohn’s disease. Further commitments of the project are the optimization of the genetic transformation techniques of the plant bioreactor and the improvement of out-of-soil cultivation techniques (University of Udine).